clinical question
- Introduction to case study, clinical question and evidence found
My Case
Mr X is an 80-year-old male who was diagnosed with Left-sided stroke. An initial computerised tomography (CT) scan of Mr X’s brain illustrated blood in the left parietal segment. A Magnetic resonance imaging (MRI) scan was conducted two days later, confirming an Ischemic infarct on the left media cerebral artery of the brain (Dobrynina et al., 2018). This infarct caused haemolysis, inability to swallow food, right side hemiplegia, which led to a lack of stability when trying to mobilise. According to the International Classification of Functioning, Disability and Health (ICF) model, the consideration of personal as well as social backgrounds is crucial in the intervention process. A review of the patient’s past background revealed that the patient lives alone in a split-level home and is mostly independent with ADLs. As a result, he experiences challenges in ascending the stairs due to the underlying stroke condition and comorbidities. History revealed an injured right hip after falling while descending stairs. As a result, the patient had hip surgery for a replacement 6/12 prior to admission. Other comorbidities contributing to the disease include hypertension, ischemic heart disease, thrombus, poor historian and difficulty making decisions (Attems & Jellinger, 2014). Patients who have suffered a stroke are faced with major challenges due to neurovascular disorders (Party, 2012). Additionally, the disorders caused by atherosclerosis, loss of blood to sections of the brain, hypertension, lack of physical movements may also result in challenging rehabilitation post-stroke. This paper will critique the evidence provided by three quantitative studies regarding post-stroke interventions.
ICF Framework for Mr X
Body Structure
- Inability to swallow food
- Pain on the hip
- Lack of balance and stability
- Muscular weakness
- Hypertension
- Ischemic stroke
- Lack of good communication
- Poor reasoning
- Balance
- Cognition
Activities (Limitations)
- Walking to and from her house
- Physical exercises
- Standing for a long time.
- Home chores (domestic activities)
- Driving
- Steps
- Personal care
Participation Limitations
- Lack of strength to take hobby activities like nature walks or athletics.
- Inability to participate in decision-based activities.
- Inability to accomplish house chores for her upkeep
- Lack of general happiness due to pain.

ORDER A CUSTOM ESSAY NOW
HIRE ESSAY TYPERS AND ENJOT EXCELLENT GRADES
Environmental Factors
- Design of the house architecture (5x stairs)
- State of living (lived alone)
- Transport options (struggles to drive)
- Access to services
Personal Factors
- Age
- Other disorders like hypertension and neurovascular disorders
- Home support
- Did you need to respond to feedback or make changes from Part A (1 minute)
Yes, I changed the Search question used as my original PICO question as it assumed a direct effect. The New PICO search question is: “What is the effectiveness of repetitive task training for stroke patient’s functional improvement, as compared to standard physiotherapy intervention” where P – Stroke, I – Repetitive task training, C – Physiotherapy interventions, and O – Functional improvement.
- Graded the papers using the NHMRC hierarchy.
- Paper 1.
Jeon, B., Kim, W., & Park, E. (2015). Effect of task-oriented training for people with stroke: a meta-analysis focused on repetitive or circuit training. Topics In Stroke Rehabilitation, 22(1), 34-43. doi: 10.1179/1074935714z.0000000035
- Paper 2.
Hubbard, I., Carey, L., Budd, T., Levi, C., McElduff, P., & Hudson, S. et al. (2014). A Randomized Controlled Trial of the Effect of Early Upper-Limb Training on Stroke Recovery and Brain Activation. Neurorehabilitation And Neural Repair, 29(8), 703-713. doi: 10.1177/1545968314562647
In paper one, evidence provided concerns patients in either of the three stages of stroke, including chronic stroke, which Mr X is found in the initial assessment. According to Jeon, Kim & Park (2015, p.36), Mr X qualified the inclusion criteria of their study, which require participants to be patients of stroke type ischemic or haemorrhagic. It also focused on walking outcomes, which is among the challenges facing Mr X. The second paper is also relevant in that it includes participants who are within their first week of initial diagnosis of ischemic stroke (Hubbard et al., 2014, p.704). However, it does not provide more details like the paper one.
The two papers have a high degree of relevance to the new PICO question. For instance, they all find the effects of task-oriented training on the movement capabilities of stroke. While they do not directly compare those effects with expected outcomes of standard physiotherapy intervention, both papers make conclusions from statistical analysis, which reduces bias. For instance, the first paper computes standard means for effect sizes from data presented in eleven articles (p.36), and the second paper used STATA version 11.0 software package to investigate differences at baseline and the change relative to baseline in the first month and the first three months (Hubbard et al., 2014, p.706).
- Discuss with your examiner key points from your evidence appraisal and application to your clinical case. (minimum of 14 minutes)
The evidence provided by the two papers is relevant to the case study since they all focus on the outcomes of repetitive task-oriented training for patients suffering an ischemic stroke. Both papers have high-quality evidence, in that the first paper is a meta-analysis of eleven articles and the second paper is a quantitative randomised trial for 23 adult patients. Both papers are consistent with their results, indicating that repetitive task-oriented training has positive effects on stroke patients.
Results obtained from the paper one was statistically significant, since P<0.05 (Jeon, Kim & Park, 2015, p.37). The second paper’s authors found a difference in brain activation to be statistically significant with P<.001. However, theydo not provide the statistically significant of their overall results, except for between-groups, where age disability, UL function, and finger tapping frequency are all statistically insignificant (Hubbard et al., 2014, p.707).
The paper one is prone to significant bias and has minimal bias reduction methods. For instance, the selection of studies was made manually through the assessment of titles and contents of abstracts (Jeon, Kim & Park, 2015, P.35). This risks the paper to increased chances of false results – a publication bias. Other bias prone to the paper are selection bias, confounding bias, and information bias. For instance, the authors only used 11 inclusion and exclusion criteria to assess their reference list titles and abstracts (p.36), but there is no warrant method for each criterion. Besides, eleven articles are not adequate to make credible conclusions. In paper two, the study comprised participants in a randomised trial with a high degree of blinding for all participants, and therapists (Hubbard et al., 2014, p.704). That reduced bias significantly. Nevertheless, that did not eliminate other biases like observational bias, which arise in a quantitative study when assessors overlook or misrecord data.

- FAST HOMEWORK HELP
- HELP FROM TOP TUTORS
- ZERO PLAGIARISM
- NO AI USED
- SECURE PAYMENT SYSTEM
- PRIVACY GUARANTEED
Regarding blinding, there was no need or opportunity to blind in paper one. However, paper two was a single-blinded longitudinal randomised controlled trial (Hubbard et al., 2014, p.703). All participants were blinded, and all assessors except concerning the objectives of the study (Hubbard et al., 2014, p.705).
The paper one does not account for any confidence intervals, while the second paper only accounts for confidence intervals in the data analysis of the UL function. The t-test, in this case had a confidence interval of 95%. This interval is critical and clinically significant, as revealed in the results section that all participants had significant improvement in their motor functioning.
In the second paper, participants from the eleven studies were clustered in three subgroups. That is, region of training and dose parameters (Jeon, Kim & Park, 2015, p.37). region training requires intensive intervention, with the lower extremities revealing increased improvement. They did not obtain data regarding dose parameters (Jeon, Kim & Park, 2015, p.41), making it impossible to compare the two groups. In paper two, intensive training group is compared to the standard care group (Hubbard et al., 2014, p.708).
The overall effect size found in paper one is ES=1.123 (Jeon, Kim & Park, 2015, p.40). The second paper does not provide the ES, but results indicate a high degree of clinical effects, as all participants showed improved health outcomes. In the first paper, nine out of the eleven studies revealed improvement, with only two indications an undefined degree of uncertainty (Jeon, Kim & Park, 2015, p.40). The second paper does not have a measure of variability, as all patients revealed improved health outcomes, as per the intensity of task orientation and brain activation (Hubbard et al., 2014, p.710).
Overall, taking results from both papers, repetitive task-oriented training has positive effects on stroke patients. Regional training would result in the lower body improving faster than the upper region, and brain activation is ideal as physical activity for increasing physical strength, speed, and balance. Both papers are barely contrastable, as the lead to similar conclusions.
The overall best evidence summary for the current PICO question is that repetitive task-oriented training is effective for functional improvement, as compared to standard physiotherapy intervention. Both papers support that the intervention has positive outcomes, with Hubbard et al. explicitly finding it better compared to standard physiotherapy (2014, p.708). Besides, the clinical size for the second paper is 1.123 – a significant effect.
Recalling the patient – Mr X, their goal is to increase their ability to climb the stairs and reduce related comorbidities. He lives alone and takes care of his ADLs. Besides, he needs to keep active to facilitate recovery of post-stroke. The strike and previous hip surgery have aggravated other health issues like hypertension and schematic heart disease.
His MID is ease to climb the stairs, and improvement in other health complications like the schematic heart disease and hypertension. This will necessitate clinically feasible hours of physical training (Hubbard et al., 2014, p.711), for instance, a six-minute timed-and-go walk (Jeon, Kim & Park, 2015, p.38). The expected effect size of walking should be a positive value to indicate progress. That is, he should have increased ease in climbing the stairs and lower blood pressure.
The intervention will cause Mr X his time and endurance to go through the repetitive task-oriented training. Some contextual factors involved are age, interests, perception, and history. For instance, the clinically feasible task must be suitable for an older adult to avoid injury (Dellinger, 2017); it should align with interest to prevent boredom, and should not aggravate former health complications. As such, one must conform to healthcare professional standards such as observing ethics and cultural competency.
Besides, the nursing team must ensure that Mr X understands the assessment, evidence, and clinical decision made by communicating effectively. The following is an example of a message communicated to him face-to-face:
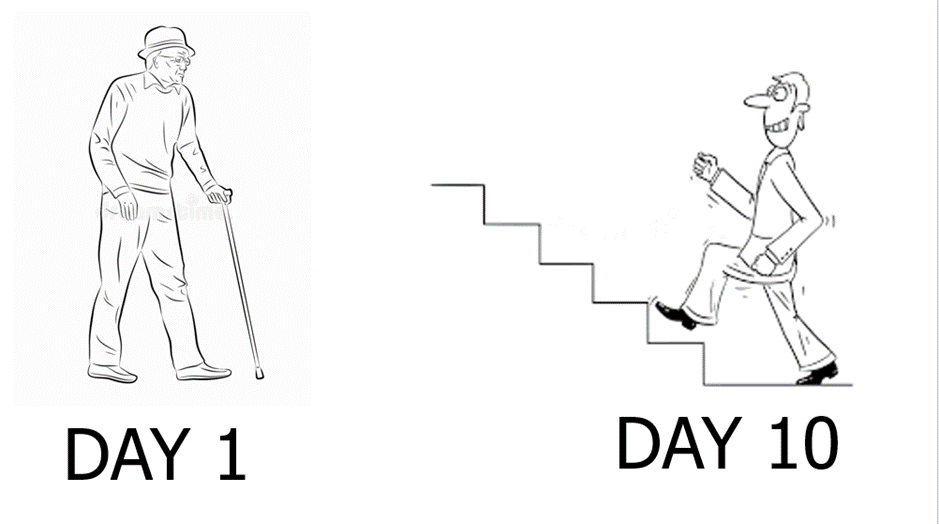
Hello Mr X. We have assessed your condition, and luckily, it is manageable. Some patients previously came to us with the same condition, and we have evidence for the exercise we shall take you through. It is a straightforward exercise, which will improve your ease to climb the stairs and increase your general body strength and balance. I can see you are eager, right? It is only walking a distance within a given time that has been approved by medical experts. This has to be done repetitively, as we shall guide you. What do you think about that? Also, you will have this poster, an illustration of the procedure. On the first day, it will feel tiring, but eventually, you will walk and climb stairs comfortably. Also, it will take your 15-30 minutes a day, in my company or a nurse assistant.
- Appraisal tools, appraise the two articles using the relevant appraisal tool
(attached)
- Grades of recommendation
Mr X is similar to the participants studied in the papers one and two. For instance, he is suffering stroke type ischemic at its chronic phase, as waling difficulties as the participants selected in the studies used by the paper one (Jeon, Kim & Park, 2015, p.35). Besides, he has once been diagnosed with a stroke, which an inclusion criterion in the paper two (Hubbard et al., 2014, p.704). However, the comparison is not adequate to sufficiently conclude that Mr X has a similar condition to the study participants.
Nevertheless, the papers one and two have significant evidence that repetitive task-oriented training is clinically feasible to improve one’s conditions against stroke. The harm is barely significant, as they include time, effort, and mental status. As such, Mr X values, which entails improving his physical strength and ease in climbing stair, align with the repetitive task-oriented training. However, his age is a limiting factor, and the task must be clinically approved to avoid injuries (Lukaszyk et al., 2016).
- Intention to treat
The limitations mentioned above and the harm are not significant compared to the beneficence, and regarding the intention to treat, there are minimal risks. For instance, the task will be facilitated by a nurse, and it shall proceed as per the clinically feasible time and size. Therefore, the treatment process shall continue after the consent of Mr X.
References
Dellinger, A. (2017). Older Adult Falls: Effective Approaches to Prevention. Current Trauma Reports, 3(2), 118-123. doi: 10.1007/s40719-017-0087-x
Hubbard, I., Carey, L., Budd, T., Levi, C., McElduff, P., & Hudson, S. et al. (2014). A Randomized Controlled Trial of the Effect of Early Upper-Limb Training on Stroke Recovery and Brain Activation. Neurorehabilitation And Neural Repair, 29(8), 703-713. doi: 10.1177/1545968314562647
Lukaszyk, C., Harvey, L., Sherrington, C., Keay, L., Tiedemann, A., & Coombes, J. et al. (2016). Risk factors, incidence, consequences and prevention strategies for falls and fall-injury within older indigenous populations: a systematic review. Australian And New Zealand Journal Of Public Health, 40(6), 564-568. doi: 10.1111/1753-6405.12585
Jeon, B., Kim, W., & Park, E. (2015). Effect of task-oriented training for people with stroke: a meta-analysis focused on repetitive or circuit training. Topics In Stroke Rehabilitation, 22(1), 34-43. doi: 10.1179/1074935714z.0000000035

